
It should be mentioned that the majority of trauma patients do not require DCR and that its techniques should be reserved for those who are the most severely injured (2). Research in military and civilian populations regarding DCR have focused on ways to improve survival in patients with severe hemorrhage. Hemorrhage secondary to trauma accounts for 40% of trauma fatalities and comprises the leading cause of preventable death in trauma (1). Accepted concepts of trauma resuscitation and surgery have been challenged in the recent wars, and novel approaches have been developed to address the current complexity and severity of not only military trauma but also civilian conflicts.ĭamage control resuscitation (DCR) has become a topic of increasing relevance and popularity over the past several years. The exact role of angiographic embolization, which should be a life-saving procedure, deserves further study.In this Euroanesthesia #EA18 lecture Bruno Pereira (Campinas, Brazil) discusses the Damage control surgery Damage control surgeryīruno Pereira, Campinas, Brazil the word “war” refer to a bad feeling it is undeniable that military conflicts have always driven innovation and technical advances in medicine and surgery. For patients who underwent angiographic embolization, mortality was 54.1%, and for those who suffered a cardiac arrest, mortality was 90%.Ĭonclusion: In blunt trauma patients with hemorrhagic shock who met criteria for the lethal triad on presentation to the ER, angiographic embolization, APACHE II score, and cardiac arrest independently predict mortality.

7.6%, p=0.01), although they had similar laparotomy rates (52.8 % vs. 14.3%, p=0.001) or an operative thoracic procedure (thoracotomy, sternotomy, or VATS, 26.4% vs. Non-survivors were more likely to undergo angiographic embolization (37.7% vs. 3232☒779 mL, p<0.001) and were more likely to have a cardiac arrest (50.9% vs. Compared to survivors, non-survivors were older (46☒2 vs. There was no difference in pre-injury comorbidities, body mass index, Injury Severity Score, multiple organ dysfunction score, ER systolic BP, ER heart rate, ER body temperature, crystalloid volume administered within 12 hours, WBC count, and platelet count between survivors and non-survivors. The mean age of the cohort was 39 years, 70% were male, and 90% were White. Results: A total of 172 patients met all three criteria. Univariate analyses were used to compare survivors and non-survivors while multivariable analysis was used to determine predictors of mortality.

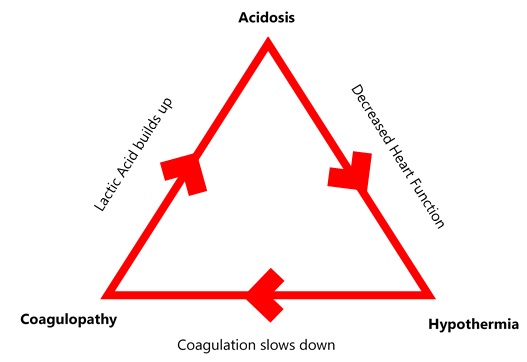
Patients who, on presentation to the emergency room (ER), had the triple combination of severe hyperlactatemia (serum lactate >4 mg/dL), coagulopathy (INR >1.5) and hypothermia (body temperature ≤ 36 ☌) were included. Methods: The Inflammation and the Host Response to Injury database was analyzed. We examine clinical variables that contribute to mortality in blunt traumatic shock patients presenting with this triad. Resuscitation and control of bleeding are two key tenets of trauma care designed to halt this vicious cycle. Introduction: The combination of acidosis, coagulopathy and hypothermia in a trauma patient is a harbinger of death. Siram 1 1Howard University College Of Medicine,Surgery,Washington, DC, USA 2Emory University Hospital,Surgery,Atlanta, GEORGIA, USA 3Northwestern University Feinberg School Of Medicine,Surgery,Chicago, ILLINOIS, USA


 0 kommentar(er)
0 kommentar(er)
